Over the past month, I have heard "co-dependency" way too often.
Somehow, the idea that supportive family and friends of people who struggle with substance use "enable" them and are "co-dependent" just won't go away.
What is wrong with the C-word?
Firstly, it is informed by the idea that addiction is a disease, which is flat out untrue. Addiction is a bio-psycho-social phenomenon with elements of oppression.
Secondly, it implies that family members and partners actively work towards keeping the user in their addiction, which, if you ask anyone who has ever had a loved one struggle with alcohol, substance abuse or an eating disorder, is very, very far from true.
Thirdly, it thereby stigmatizes not only the user, but also their support system as defective, when really, the opposite is true. Time and time again, stigmatizing people and calling them names has proven to be harmful and produce adverse effects.
Someone who is working hard at keeping their loved one safe deserves praise, not contempt.
What is, unfortunately, typically called "enabling behaviour" - providing people with love and attention, a place to live, perhaps Naltrexone and an opportunity to safely use drugs, for example - are really evidence-based strategies that we know to use in publicly funded harm reduction efforts: They significantly reduce the number of overdose deaths and actually help people who struggle with problematic substance use cope better in life.
Whether we are talking about people in recovery from eating disorders or substance use - the tough love approach doesn't work. Instead, family-based treatment is recommended wherever possible. In fact, it doesn't matter which or how many family members show up, as long as they do, even if the person who is struggling is the only one NOT attending counselling.
Why? Because it has been shown that there is a ripple effect of positive change within social systems.
And here is another important aspect of the debate:
Most often, caregivers are women. Labelling them as cognitively defective for fulfilling the role that society forces on them is devaluing and anti-feminist.
Expecting wives, lovers, mothers, sisters, aunts, and best friends to detach from from their partners and children in distress, while at the same time being "good" and "respectable" women is asking the impossible.
Of course, family members are not typically trained in addictions counselling, and even when they are, they are ill-equipped to counsel loved ones.
Rather than casting blame, we should utilize the knowledge and support loved ones can offer for the benefit of treatment.
Just like people who display what we would consider problematic behaviours, their family members already feel bad enough. Labelling and stigmatizing them will not help, but rather perpetuate the problem.
As practitioners, we are in the best possible position to talk with people rather than about them.
Warmly,
Annina Schmid
Cannabis Use In Pregnancy Isn't Safe
I recently attended an excellent presentation on substance use in pregnancy, which was held by Dr. Erin Lurie, addiction medicine fellow at the University of Toronto and staff member at the Substance Use in Pregnancy Clinic (SUP) at St Michael’s Hospital.
Dr. Lurie's presentation was part of a series of educational events called Addiction Rounds facilitated by CAMH.
If you are interested, you can find out more about these and similar events through the EEnet connect events calendar.
Of the issues that Dr. Lurie discussed, I personally found her research update on cannabis use in pregnancy most fascinating.
With the pending legalization of Cannabis in Ontario, I thought it could be helpful to share some of her findings in this newsletter.
Below, please find an interview with Dr. Lurie on substance use in pregnancy and while breastfeeding:
Dr. Lurie, as someone who is directly involved in medical work with women who use alcohol, cannabis or heroin in pregnancy and while breastfeeding, what is the most important thing you would like us to know about your area of expertise?
The most important thing to know is that any active substance use in breastfeeding has the potential to be harmful. It sounds like a bit of a hard line, but the risk is really both with the exposure of the specific substance through the breastmilk as well as the risk of caring for a young newborn and infant while intoxicated. While we do not have great Canadian guidelines on substance exposure and breastfeeding, the American Academy of Breastfeeding Medicine has excellent guidelines on the issue.
Thank you for pointing that out. In my experience, most people focus on substance use during pregnancy and hardly ever talk about substance use when breastfeeding - other than, perhaps, when they try to play down the risk of alcohol consumption during that time. Specifically with regards to cannabis use, what is it that people need to be aware of in this context?
With the upcoming legalization of cannabis it’s important to point out that there is NO safe timeline after use for exposure with breastfeeding.
Meaning that even if we were to smoke at the end of the day, it would not be safe to breastfeed the next morning?
Correct. THC is the psychoactive component of cannabis. It stays in the body for a very long time: up to 48 hours in infrequent users, and in chronic users or people who use nearly daily even up to four days. THC also likes to store in fatty tissue, and breast milk, especially early on, is very very fatty. THC has been shown to be concentrated in breast milk and be up to eight times the amount that would be in the same person’s bloodstream.
Wow! And with regard to cannabis use in pregnancy - what would you tell those that advertise cannabis as anti-nauseant?
Well, we know that both the Society of Obstetricians and Gynaecologists of Canada, as well as the American College of Obstetricians and Gynaecologists recommend to abstain from cannabis use during pregnancy in their 2017 guidelines. This is because it has been shown that some of the risks of prenatal exposure to cannabis include decreased fetal growth, preterm birth, miscarriage, stillbirth, and significant long-term neurobehavioural changes. The latter have been documented by the Canadian Centre on Substance Use and Addiction [see infographic below] and can impact children and young adults up to 22 years of age.
So, when we compare all of this to the effects of opiate replacement therapies during pregnancy and while breastfeeding, is it safe to say that the negative effects of alcohol or cannabis use are actually much worse for the child, both long-term and short-term, than, say of Methadone?
Correct. In the absence of any other substance use, opiate replacement therapy - including Methadone and Suboxone - is very safe, and even protective to prevent neonatal abstinence syndrome (the withdrawal a baby experiences when they are no longer exposed to opiates from the mom after delivery). For women who are stable in their recovery from opiates, breastfeeding is encouraged.
Thank you so much for taking the time to answer these questions, Dr. Lurie.
As always, I hope this article has been helpful to you.
Warmly,
Annina Schmid
The Substance Use in Pregnancy Clinic (SUP)
at St Michael’s Hospital is open to referrals:
St. James Town Health Centre
410 Sherbourne St., 1st Floor
416-864-3082
Open Wednesdays 12:00 – 4:00
Using a multidisciplinary health care model, the clinic helps to support women with previous or active substance use throughout their pregnancy
Patients can be seen within the week and can drop in for their first appointment.
Please email either Dr Lurie (luriee@smh.ca) or Dr Turner (turnersu@smh.ca) for referrals of pregnant patients only.
New FREE Webinar: Intro To Intuitive Eating
You guys, I cannot even contain my excitement for this FREE webinar that Sarah Berneche (Anti-Diet RHN and certified Intuitive Eating Counsellor) and I have recorded yesterday!
I am not kidding when I say this should be mandatory viewing for absolutely everyone who has ever thought twice about food - I promise you will not be disappointed.
What we talk about here is exactly what we talk about in session with clients (minus, of course, the individualized care and support).
If you are willing to dedicate about an hour of your time anytime after September 3rd, this is an excellent way to spend it.
Simply register your name and email address here and wait for the thing to be delivered to your inbox on Monday, September 3rd, at 12pm EST. (Feel free to share this email or link with your friends and colleagues, too!)
This is the first of a few upcoming webinars this Fall, and I will keep you posted about all of them, of course. <3
The Recovery Benefits Of Filtered Messages
Aligning our actions and speech with our true feelings and thoughts will work wonders in recovery.
In today's blog post, I want to focus on a difficult scenario - such as an argument with someone we like - and how we could handle that in recovery.
Most likely, when we're in a bad place with ourselves, we tend to accuse and blame others in arguments.
Or maybe we're the type of person who chooses to walk away from unpleasant exchanges.
Whether we argue or take off, though, there will come a moment after the fact when we will be alone with our feelings.
Most probably, we won't feel too great about how we handled ourselves.
We might feel extra bad, because we were being hurtful on purpose.
Enraged, we might have said exactly what came to our minds, unfiltered and fuelled by disappointment or resentment.
Or, if we chose to walk away, we might feel worse, because the problem at hand is still unresolved.
Another Approach: The Filtered Message
As a third option, aside from sharing unfiltered opinions and walking away from discomfort, I would like to introduce the filtered message.
Filtering our messages is often helpful to our own peace of mind, and with that especially important in recovery.
Here are the basics of a filtered message, as explained in the following example:
Tom has an argument with his partner Tim, during which Tim makes unfair assumptions. Tom is getting angrier and angrier, as Tim's comments hurt his feelings. Instead of leaving the situation without comment, which is the other idea that comes to Tom's mind, he decides to give Tim a piece of his mind:
"You have no proof for any of this! Why do you keep making things up? You're an a*hole, Tim!"
These are the thoughts that came to Tom's mind, exactly how he heard them in his head. Without thinking much, and because he was hurt, Tom attacks Tim back. The argument continues for a little while, with both of them cussing each other out and Tom leaving to get a drink at the bar in the end.
Had Tom chosen to send a filtered message instead, it could have read something like this:
"I don't like listening to your accusations. They're untrue, but I don't have the energy to fight them at the moment. I will go home now, because I need space."
Tom would have left the scene, upset, but proud of the fact that he was able to speak his truth in a way that did not perpetuate the argument.
Think about a recent scenario where you said something unfiltered, and try to think of a filtered way to state how you felt, and how you could handle a similar situation going forward.
It's important that your filtered statement focuses only on you and your experience of the moment; without casting blame on your partner, and also without passive-aggressive undertones.
Why are filtered messages helpful to your recovery?
Filtered messages are helpful to your recovery, because:
- You won't have to "get rid of" bad feelings through problem behaviours, as there will be fewer or even no bad feelings at all after making a filtered statement
- You will learn how to speak your truth in a way that is the least hurtful to people while staying true to yourself
- You will get more comfortable with speaking your truth
Hope this was helpful!
What Type Of Person Makes You Feel Most Comfortable?
One thing I love about facilitating online groups is that so many interesting thoughts and view points are expressed by participants that lead to new insights for everyone.
Most recently, the issue of going out for dinner came up, and how that can make those of us struggling with disordered eating or body image issues very uncomfortable.
(You could easily make up a similar scenario for someone trying to stay sober when all their friends are still drinking - navigating going out is *hard* in the beginning!)
In our group discussion yesterday, we came to see that there tend to be two types of people:
Those who make us feel comfortable around food (or are okay with us not drinking) and those who don't or do so less (or aren't).
My question for you tonight is:
What type of person does it take to make you feel relaxed?
No matter whether around food or in other anxiety-provoking social situations.
What are their qualities, behaviours and attitudes?
List at least three features of the person that puts you most at ease. If you don't have such a person in your life at the moment, make one up: What would they need to say or do so you could feel calmer?
Lastly, if you can at all, surround yourself with those helpful actions and attitudes more often. <3
Talk soon,
Annina
Self-Compassion vs. Self-Criticism
Today I wanted to provide you with two little thought experiments to try at home:
One revolves around your needs, the other around your thoughts.
Both are easy to try whenever you remember to do so.
Choose your choice!
The first one goes like this:
When someone asks you what you would like to do, see, try, etc., try not to respond with "I'm easy", "You choose", or "I don't care either way."
Instead, take the question seriously and try to really think about which option you would prefer.
Then, state your preference and see what happens!
Self-Criticism vs. Self-Compassion
The second experiment is a little more subtle, but even more important.
Pick literally any event, instance, or situation that happened to you today or yesterday, and compare and contrast two reactions to it:
The self-critical response vs. the self-compassionate response.
Try it:
Let's say you missed the bus.
The self-critical way of thinking would go something like:
"Why am I always late?! This is the third time in the last couple of weeks that I took too long to get out of bed in the morning. Everybody else has their act together and I'm the only one who can't even leave the house at the right time!"
Not so nice, is it?
Now try the self-compassionate response instead:
"Ok, I missed the bus again. I guess I must be really exhausted, considering how hard it is for me to get out of bed at the moment. I really deserve a break. Perhaps I could take some days off?"
So much kinder!
And the best part is:
This works with literally any situation.
Have a kind day and talk soon,
Annina
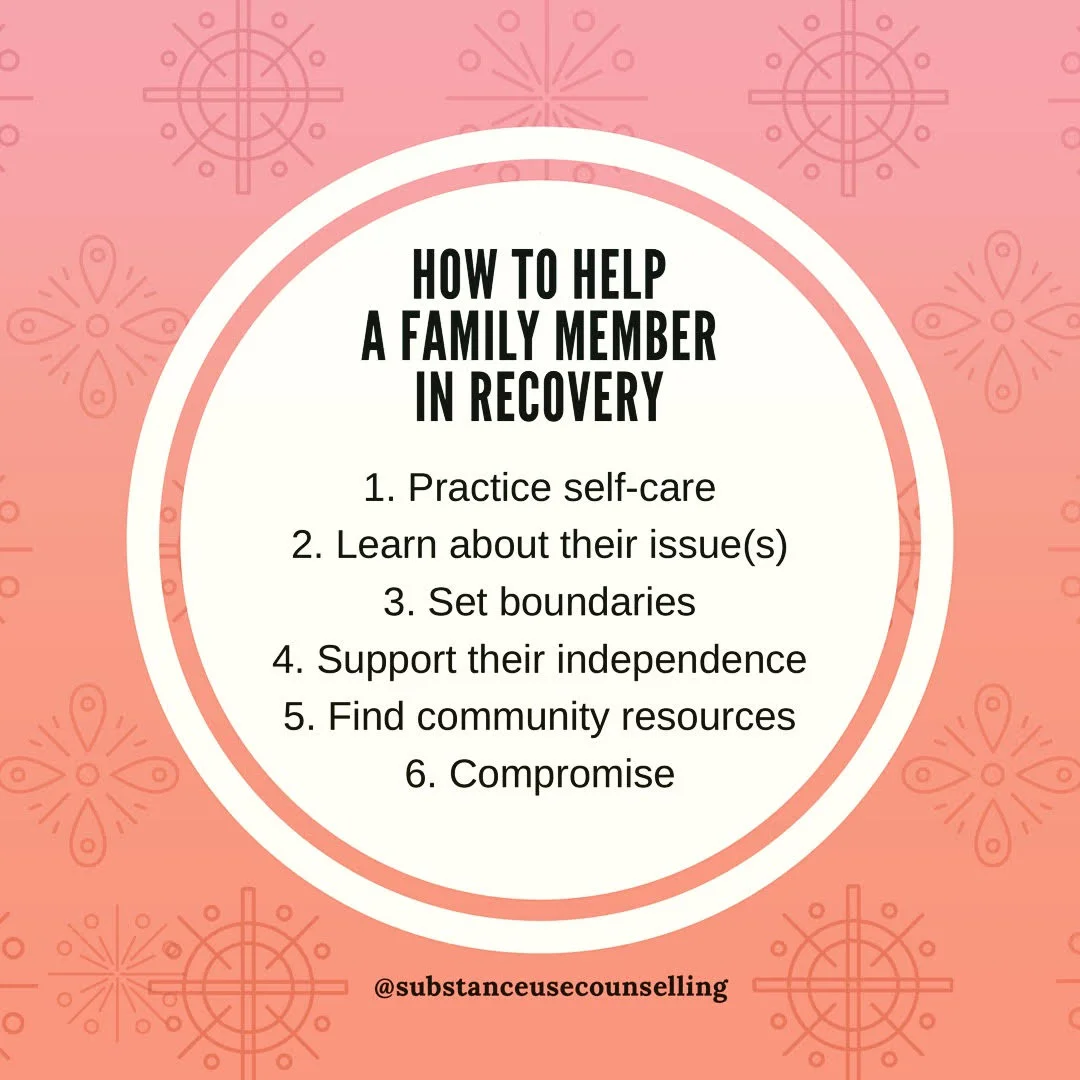
How To Help A Family Member In Recovery
What to do when one of your family members, a partner or close friend is struggling with an addiction or eating disorder?
You might be surprised to hear that about one third of my clients are not personally in recovery, but coming to see me because they want to learn more about, for example, how growing up with a person who drank problematically impacts them every day as an adult.
Or why it is so hard to see a sibling smoke too much weed.
Or why their sister's eating disorder just won't go away.
I touched briefly on this topic in one of my last emails to you, The Role of Siblings.
What I didn't mention in that email is how important family support is in recovery. It is very, very important.
In fact, the importance of family support in recovery cannot be stressed enough.
Treatment outcomes are much better when even just one family member other than the person struggling agrees to seeing a counsellor, too.
They could see a different counsellor, or the same one, and could come to sessions together or separately - any involvement has proven to be more effective than no involvement.
And the more family members participate, the better!
Ok, so aside from joining the family member in recovery in seeing a counsellor, what can we do when a loved one is struggling?
Try the following six steps:
- Before all else, make self-care a priority.
- Learn about the substances and mental health problems your loved one struggles with.
- Don't let them abuse or hurt you or put you in danger. Ever. (If this is difficult for you, consider attending my boundaries workshop on November 14th in Toronto.)
- Help your affected family member become as independent as possiblein everyday life.
- Guide them towards appropriate community resources and treatment options and help them make use of those as best as you can - for example by becoming an accountability partner.
- When disagreement arises about which next step to take, work towards a compromise and find a way forward that all family members can agree with - including the member who struggles.
Let me know if you have any questions about these steps, I would be happy to answer them.
And if you have a friend who could find this information helpful, please feel free to forward it to them, too.
Webinar Replay Now Available!
This is just a quick note to let you know that the replay of the free webinar I recorded last week is now available - all you need to do to watch is click the link.
I know it says that it's for parents, but that's really not true - any woman who has struggled with emotional eating or binge eating will be able to relate to the content of our discussion and hopefully also gain some new insights around not only why diets don't work, but why they are flat out harmful.
At the beginning, Olivia - whom I would hire as postpartum therapist any day, by the way - talks a little bit about her own traumatic experience with dieting (it literally almost killed her... consider this your trigger warning!).
Then, we dive right into the mindfuck that is living in a culture that wants to make money off our fear of being or becoming fat.
The struggle is real!
If you're interested in how Olivia and I approach those subjects, feel free to watch us in action here.
And if our talk raises further questions for you, do let me know, I'm always happy to help.
Talk soon,
Annina
P.S. Do you know another woman/ mom/ caregiver who might be interested in this webinar? Please feel free to share the feminist love and forward them this email. <3
How To Train Your Resilience Muscle
** This is a transcript of a brief video I posted recently: "How To Become More Resilient" **
Today, I want to briefly talk to you about resilience.
How come some people are more negatively affected by bad stuff happening in their lives than others?
Well, we know that two things impact how resilient we are.
One of them is luck. (Okay, can't do anything about that!)
But the other one is actually how in control of our lives we feel.
If we are under the impression that we are an agent in what we do, and we can actually positively influence what's happening to us, we're more resilient than when we don't feel any kind of agency in our lives.
The good news is that resilience can be learned!
It has so much to do with how we frame and conceptualize events that happen to us.
Next time something not so great is going on in your life, ask yourself how you see this event.
Is this something traumatic and horrible that's happening to you?
Or is this an opportunity to learn and grow?
Easier said than done, but worth a try, isn't it?